GENERAL MEDICINE
July 15,2023.
General Medicine.
Case scenario,
Hi, I am Aishwarya, 3rd bds student. This is an online elog book to discuss our patient health, data after taking his consent. This also reflects my patient centered online learning portfolio.
Case history
Patient details
A 62 yr old male saree weaver by occupation presented with,
Chief complaints
Pedal edema since 6 months,
Decreased urine out put since 1 month
Vomitings since 15 days
Shortness of breath since 2 days
History of present illness
Patient was apparently asymptomatic 10 months back, then he started developing low sugar levels, he visited a local and then sent to a test and diagnosed as renal failure and treated accordingly.
Since last 1 month he complaints of decreased urine output, and vomitings since 15 days which is non projectile, non bilious, food particles as content, non blood tinged.
Also complaints of shortness of breath since 2 days, grade 2, relieved by rest also has a facial puffiness since a week.
History of past illness
15 yrs back he was diagnosed as diabetes mellitus type 2 and on medication.
Hypertension since 3 yrs
Tuberculosis since 5 yrs
Also diagnosed with CKD since 1 yr
No asthma
No CVA
No epilepsy
Personal history
Appetite decreased
Diet mixed
Sleep nrml
Bowels decreased
Micturition decreased
Habits.
Alcohol consumption but stopped 5 yrs back
No history smoking.
Family history.
Not significant
General examination
Pt. Is consious , coherent and co operative
Pallor : present
Icterus : no
Clubbing: no
Lymphadenopathy: no
Cyanosis: no
Pedal edema : present
Drug history:
Amlodipine 10mg
OHA medication.
Systemic examination:
Abdomen: soft and non tender
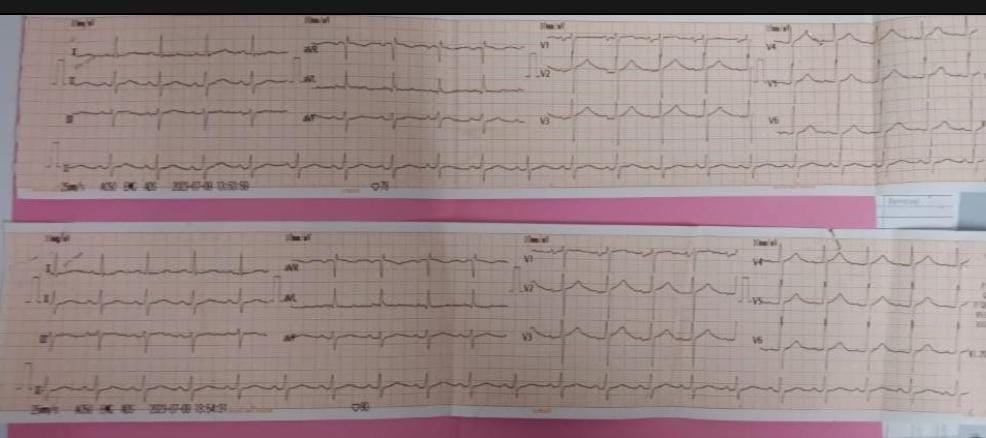
CVS: no murmurs
Respiratory system: normal
Vitals:
Pt. Is consious
Temperature: 96.8F
Respiratory rate: 20cpm
Pulse rate : 80 bpm
Blood pressure: 170/80 mmHg
SpO2: 90
Provisional diagnosis:
AKI on CKD



Comments
Post a Comment